Cornea, Cataract, IOL
Cataract Surgery in Eyes with Corneal Disease
Applying information from preoperative diagnostics guides surgical planning.

Cheryl Guttman Krader
Published: Monday, February 3, 2025
“ The effect of a diseased cornea on outcomes of cataract surgery is an important topic considering the cornea accounts for more than 60% of ocular power. “
Cataract surgeons operating on eyes with corneal disease need to understand how different abnormalities impact quality and quantity of vision, said Damien Gatinel MD, PhD.
“The effect of a diseased cornea on outcomes of cataract surgery is an important topic, considering the cornea accounts for more than 60% of ocular power,” Dr Gatinel said. “Power is not everything, however, because a diseased cornea also affects optical quality.”
Modelling with a new device that uses interferometry technology and wavefront propagation aberrometry to analyse the optical quality of IOLs (NIMO TEMPO, Lambda-X) allows insight into the interactions between different corneal abnormalities and different IOL optic designs.1 Dr Gatinel illustrated this point with a series of examples showing how modulation transfer function, point spread function, and depth of focus can be dramatically affected in eyes with keratoconus or different amounts of corneal spherical aberration compared to those with a ‘normal’ cornea.
“The consequences for postoperative visual performance are important to keep in mind during our surgical decision-making,” he explained. “But there is another problem cataract surgeons face when operating on eyes with a diseased cornea: the issue of IOL power.”
Understanding of the latter issue is gained through evaluations performed with different types of diagnostic instruments, and Dr Gatinel highlighted this point by discussing another group of cases. In one example, he showed wavefront analysis and corneal topography imaging would predict poor visual acuity after cataract surgery in an eye with keratoconus where there is power distortion from the anterior cornea.
“Putting a contact lens on the same eye results in improved visual acuity, which confirms the cornea is the cause of the problem,” he said. “It also indicates the contact lens will do a better job correcting this patient’s vision than any toric pseudophakic IOL.”
As further support for his point, Dr Gatinel presented a case of a keratoconic eye implanted with a toric IOL. Although the measured refractive outcome was good, the topography and wavefront analysis showed a vertical gradient of uncorrected power due to persisting coma asymmetry (see image).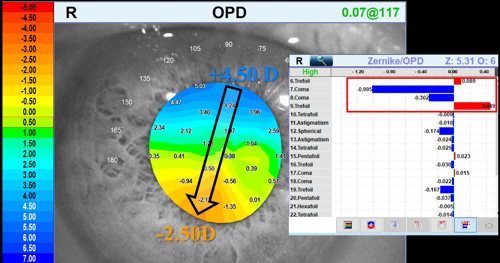
“I dare anyone to [guess] the refraction of that eye in which there is a 7.0 D power change from the top to the bottom of the pupil,” he said.
Dr Gatinel also discussed the evaluation and management of eyes with a loss of corneal transparency that can occur because of dystrophies, haze, scarring, or oedema. He recommended measuring light scatter in these cases to assess the potential impact on post-cataract surgery visual quality, mentioning a recently published paper describing an objective approach for detecting subclinical oedema developed by applying artificial intelligence to the analysis of corneal OCT images.2
A final case involved a patient with extreme corneal opacity and aniridia who was able to function until a cataract developed. Given the situation, Dr Gatinel said he was reluctant to perform either cataract surgery or a corneal transplant. Ultimately, he proceeded by trephining the cornea, removing the cataract, implanting an IOL, and replacing the trephined tissue.
“Postoperative BCVA was dramatically improved to 20/200, which allowed the patient to function without dependence,” he said. “The lesson I learned from this case is it is still worth removing an opaque crystalline lens in an eye with an opaque cornea because having two opacities is still worse than one.”
Dr Gatinel spoke during Cornea Day at the 2024 ESCRS Congress in Barcelona.
Damien Gatinel MD, PhD is Head of Anterior Segment and Refractive Surgery, Rothschild Foundation Hospital, Paris, France. gatinel@gmail.com
1. Stern B, Saad A, Flamant R, Joannes L, Gatinel D. “Intra-observer and inter-observer variability of intraocular lens measurements using an interferometry metrology device,” Diagnostics, 2024; 14(2): 216.
2. Zéboulon P, Ghazal W, Gatinel D. “Corneal edema visualization with optical coherence tomography using deep learning: proof of concept,” Cornea, 2021; 40(10): 1267–1275.
Tags: Barcelona, 2024 ESCRS Congress, keratoconus, cataract surgery, diseased cornea, corneal disease, IOL, Damien Gatinel, corneal abnormalities, abnormal corneas, topography, corneal topography
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.